On March 10, 2021, Andrée Dubord was taken to a hospital in Quebec City. Diagnosed with colon cancer, she was told by doctors that she must undergo surgery and after that would have to live with a colostomy bag that would need to be emptied each day. Declining the operation would mean serious complications, including fecal vomiting. That evening she turned down both options and applied for medical assistance in dying.
The next day, Laurence Godin-Tremblay, her granddaughter, was at her bedside when a doctor strode into the room. “11 a.m. tomorrow?” he suggested.
Ms. Godin-Tremblay was stunned to learn that her 89-year-old grandmother was being scheduled to receive aid in dying in just a few hours. The doctor explained to family members that Ms. Dubord’s application had been rapidly accepted and approved and that the speed of the decision was intended to alleviate the patient’s “fear of suffering.”
“It has become increasingly common for a patient to apply for medical assistance in dying, get approved and receive the procedure on the same day, all within a span of 24 hours.”
The following morning Ms. Dubord passed away after receiving a lethal injection. In an entry in a book of condolences left for the family, one of her friends wrote that Ms. Dubord “didn’t want to disturb anyone.”
Ms. Godin-Tremblay wonders if the loneliness her grandmother felt during the Covid-19 pandemic contributed to her decision to seek assistance in dying. Almost two years later, she still struggles to mourn the loss of her grandmother. Describing herself as one of the few members of her family who is a practicing Catholic, she believes she is also one of the only family members to feel unease about the circumstances of her grandmother’s death. Everything happened too fast, she said.
Medical assistance in dying in Canada, known by its abbreviation MAID, “was [first] proposed as an exception,” said Ms. Godin-Tremblay, a professor at the seminary for the Archdiocese of Montreal who is completing her doctorate in philosophy. Now, “even my 19-year-old brother said he was going to apply for MAID when he gets old. It’s becoming the norm, as if it’s the new way to die.”
The rush to the conclusion of an assistance-in-dying application experienced by her family is not unique.
“It has become increasingly common for a patient to apply for MAID, get approved and receive the procedure on the same day, all within a span of 24 hours,” said Leonie Herx, an associate professor of palliative medicine at Queen’s University, during hearings in 2022 of the Parliament’s Special Joint Committee on Medical Assistance in Dying.
A new way of dying?
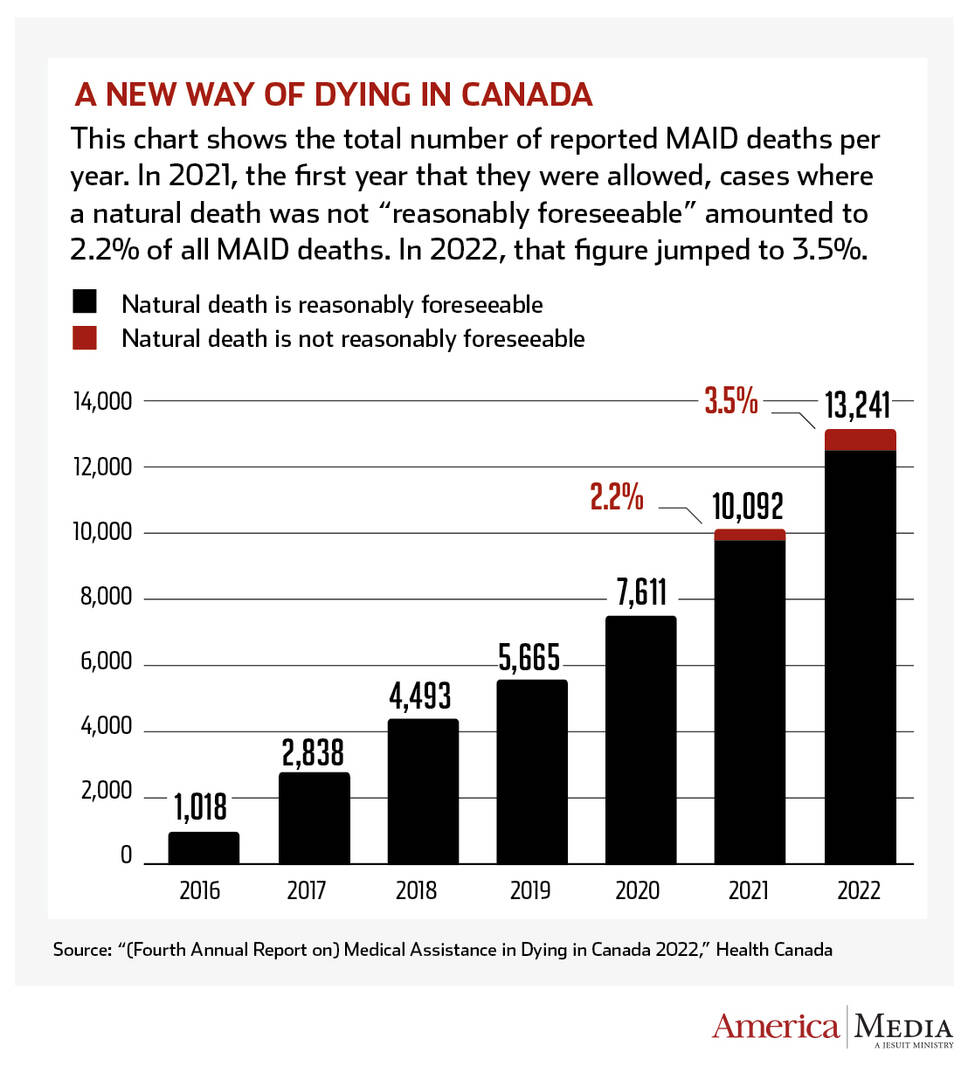
The number of deaths under MAID has increased steadily since assistance in dying was decriminalized in 2016. And the number of MAID approvals may well continue to rise, given a recent broadening of eligibility for aid in dying.
The following morning Ms. Dubord passed away after receiving a lethal injection. In an entry in a book of condolences left for the family, one of her friends wrote that Ms. Dubord “didn’t want to disturb anyone.”
Assistance in dying was originally limited to adults experiencing intolerable suffering, whose condition was characterized by an advanced and irreversible decline in capacity and who were on a trajectory to natural death. But in 2021, Canadian legislators extended eligibility to people whose natural death was not reasonably foreseeable.
On March 17, 2024, after several postponements, individuals suffering with mental illness will also become eligible to apply for MAID. And in the province of Quebec, a new law intended to be implemented by 2025 expands access to aid in dying for individuals with severe physical disabilities or major neurocognitive disorders, like Alzheimer’s disease, who will be allowed to make “advance requests” for MAID.
“New ethical issues are emerging with each expansion of the law,” said Jasmin Lemieux-Lefebvre, coordinator of the advocacy network Vivre Dans la Dignité (Living in Dignity). “There is a lack of consensus regarding the inclusion of mental disorders in MAID. Various experts are raising concerns and saying, ‘We’re not ready at all [for the broadening of the law] with the waiting time for mental health care.’” He explained that Canadians seeking psychological services may have to wait many months before receiving help.
The Canadian Conference of Catholic Bishops has denounced these latest expansions of MAID eligibility, particularly the inclusion of people suffering from mental illness.
In an open letter to the Canadian federal government last May, the Canadian bishops said: “It is even more objectionable when the government extends euthanasia/assisted suicide to individuals whose mental condition may predispose them to suicide, especially since it is known that health care across Canada is failing to provide accessible and reliable treatment for patients living with mental health challenges including mental illnesses. To enable or assist in the suicide for these patients directly contradicts national suicide prevention strategies and reneges on our collective social responsibility.”
Laurence Godin-Tremblay wonders if the loneliness her grandmother felt during the Covid-19 pandemic contributed to her decision to seek assistance in dying. Almost two years later, she still struggles to mourn her loss.
The issue is likely to remain contentious for the church in Canada. Supporters of assistance in dying are planning a court challenge that would oblige government-funded Catholic medical facilities to perform assistance in dying on site. The current practice allows MAID patients to be transferred to other institutions before the lethal procedure.
A survey in October found that 58 percent of Canadians believe that religiously affiliated institutions should not be required to provide MAID services, but it also found less support for expressions of individual conscience among health care providers. Seven in ten say a doctor morally opposed to MAID should be required to make a referral if a patient asks for a medically assisted death.
Health ethicists in Canada are beginning to raise questions about the thoroughness of MAID oversight and mechanisms to protect vulnerable populations. Many are concerned that the limited capacity of mental health services and lack of housing and other social supports seem to have been the primary drivers of decisions to seek aid in dying.
“Since Bill C-7,” an amendment that expanded eligibility, “we’ve seen countless cases in the media and in our doctors’ offices of individuals seeking and obtaining Medical Aid in Dying because they can’t access essential [social] support, including palliative care, home care and care for people with disabilities,” Dr. Herx said. “There are significant disparities in access to palliative care across the country, especially in rural and remote areas.”
Dr. Herx testified that only about half of Canadians have access to the palliative care they need and said that the quality of that care remains uncertain. “Currently, Canadians are entitled to medical assistance in dying, but not medical assistance in living,” she said.
Supporters of assistance in dying are planning a court challenge that would oblige government-funded Catholic medical facilities to perform assistance in dying on site.
Trudo Lemmens, who holds the Scholl Chair in Health Law and Policy at the University of Toronto’s law school, is deeply concerned about how MAID has been instituted. “What we’ve seen in Canada is unique in the world,” he said. “Canada is an example of how the [assisted suicide] system can derail.”
According to Mr. Lemmens, the expanded federal law and various policies that established the aid in dying process reflect a misleading interpretation of the Supreme Court’s decision in Carter v. Canada, which in 2015 opened the door to assistance in dying, as if it created a broad constitutional right. They send a message to patients and people suffering from chronic ailments in Canada, he argued—a notion that “medical assistance in dying has become a therapy for all kinds of suffering.”
“We’re starting to normalize the [assisted] end-of-life as a solution to problems that could be approached differently,” he said. “Ending someone’s life can be cheaper than providing timely access to quality mental health care and quality home care. [But] there is something deeply problematic when society, including philosophers, justifies [assistance in dying] as a form of compassion and relief.”
He argued that Canadians need to confront the weaknesses being exposed in its social safety net, especially for vulnerable populations like people who face disabilities or mental illness, or Indigenous communities, which experience high rates of suicide.
In the province of Quebec, where Ms. Godin-Tremblay and her family live, the proportion of people opting for MAID in 2021 far surpassed rates for assisted suicides derived from other laws around the world.
In 2022, more than 13,000 people received assistance in dying in Canada, accounting for 4.1 percent of all deaths, an increase of over 30 percent from 2021.
California, a U.S. state with a population comparable to Canada’s, also legalized an end-of-life option in 2016, but the number of deaths carried out under the California statute has remained constant at around 0.15 percent of deaths in 2020 and 2021. (According to the California law, terminally ill adults may obtain and self-administer aid-in-dying drugs.) Over the same period, the total number of assisted deaths in Canada rose from 2.5 percent to 3.3 percent of all deaths. In 2021, just 486 individuals ended their lives under the California law while 10,064 Canadians died under MAID.
In 2022, more than 13,000 people received assistance in dying in Canada, accounting for 4.1 percent of all deaths, an increase of over 30 percent from 2021. In Quebec, MAID accounted for almost 7 percent of deaths between April 1, 2022, and March 31, 2023.
In two administrative regions of Quebec, MAID accounted for almost 10 percent of deaths, according to the Commission on End of Life Care, a provincial body responsible for overseeing the implementation of MAID. A spokesperson for the commission declined to speak with America until a study of the social impact of MAID is completed in 2024, but in 2023, the commission issued alerts to physicians who offered aid-in-dying services, reminding them that “advanced age and issues related to aging are not considered serious and incurable diseases and do not warrant MAID.” Approval for assistance in dying requires the signatures of two experts, and the commission also reminded providers that “shopping around for a second favorable opinion is not an acceptable practice.”
A lack of access to care
As the number of MAID approvals mount, they have been accompanied by many cases that raise concerns. Last June, The Globe and Mail reported the case of a 37-year-old woman who was experiencing frequent episodes of depression and suicidal thoughts.
She sought counseling at a hospital in Vancouver, where a clinician told her she would have to wait months for treatment. Suggesting that the mental health system in the province was “broken,” the clinician then asked if she had considered applying for assistance in dying. (Hospital officials confirmed that the discussion took place but said the topic of aid in dying was raised to gauge the patient’s risk of suicidality. The patient said mentioning the issue merely heightened her distress.)
Health ethicists in Canada are beginning to raise questions about the thoroughness of MAID oversight and mechanisms to protect vulnerable populations.
Denise, a woman in her 30s with physical disabilities who also suffers from a condition known as multiple chemical sensitivities, requested assistance in dying in 2022 after unsuccessful attempts to find affordable housing in Toronto that could accommodate her health needs.The young woman abandoned her application after a crowdfunding campaign raised some money to assist her. Unfortunately, Denise is still struggling to find appropriate housing and reports that she is considering reapplying for MAID.
In an article published in the medical journal Palliative and Supportive Care in 2023, four medical and ethical experts discussed a number of problematic experiences related to MAID. A former soldier and Paralympics participant from Quebec, Christine Gauthier, has been trying for five years to have a wheelchair ramp installed at her home. She testified that her caseworker from Veterans Affairs Canada suggested aid in dying instead of the home modification.
At least four other veterans were similarly offered aid in dying during discussions of assistance from V.A.C., the office of the minister for veterans affairs told media. According to the office, V.A.C. staff have been reminded that discussions about MAID are “not the place of Veterans Affairs Canada.”
Alan Nichols, who suffered from a hearing and cognitive disability, had been experiencing recurrent episodes of depression. He was able to apply for MAID. His family was informed just four days before his assisted death but were unable to persuade officials to halt the procedure. The Associated Press reports that his MAID application listed only one health condition as the reason for his request to die: hearing loss.
Sathya Dhara Kovac, who at 44 had been living with amyotrophic lateral sclerosis, hoped to carry on but opted for aid in dying because of a persistent struggle to receive home care assistance. She wrote her own obituary before accepting aid in dying. “Ultimately it was not a genetic disease that took me out,” she told loved ones, “it was a system…. Vulnerable people need help to survive. I could have had more time if I had more help.”
None of these cases were flagged in Health Canada’s internal reports as worrisome, according to the authors of the review Palliative and Supportive Care. They report that in Canada there is no reliable system for objectively or retroactively uncovering any errors or abuses in how assistance in dying is being practiced.
Asked about the risks of abuses in assistance in dying, a neurosurgeon and president of the Quebec Association for the Right to Die with Dignity, Georges L’Espérance, remains a confident supporter of the practice. “Considering the advancements, [the process] is completely fair, ethical, moral and legal, as long as we don’t let religious concepts hinder us,” he told America.
Most patients who pursue assistance in dying, he feels sure, have decided: “‘I’ve lived my life, I no longer find any joy in it.’ How can we justify ending life in suffering, pain and decay?”
But Ms. Godin-Tremblay is left wondering about contemporary Canada’s attitude toward life and death. “We live in a society where the weakest are seen as troublesome,” she said. “My grandmother had expressed her desire not to disturb people, and she made up her mind a long time ago. But she wouldn’t have bothered me. I would have liked to have been there for her.”
MAID In Canada
- 13,241 medical assistance in dying provisions were reported in Canada, accounting for 4.1% of all Canadian deaths in 2022, more than 31% higher than numbers reported in 2021.
- 4,801 Quebec residents in 2022 opted for a doctor-assisted death—a 46% increase from 2021.
- 6.6% of all deaths in Quebec in 2022 were from MAID—the highest rate in the country and the highest rate for assisted suicide in any jurisdiction in the world.
- 77—the average age of individuals at the time MAID was provided.
- 63% of MAID recipients in 2022 said cancer was their underlying medical condition, the most cited cause for seeking MAID.
- 44,958—the total number of medically assisted deaths reported in Canada since the introduction of federal MAID legislation in 2016.
- Medical aid in dying, first established in the United States by the Oregon Death with Dignity Act in 1994, is legal in 10 states—California, Colorado, Hawaii, Montana, Maine, New Jersey, New Mexico, Oregon, Vermont and Washington—and the District of Columbia.
Source: “(Fourth Annual Report on) Medical Assistance in Dying in Canada 2022,” Health Canada
Correction: The timeline for the lifting of the prohibition of assistance in dying was depicted incorrectly in the original version of this report. Federal expansion of the protocol followed a court decision in 2015. The court was not interpreting new law as originally reported. The error has been corrected. Trudo Lemmen’s position at the University of Toronto was also misstated. He is the Scholl Chair in Health Law and Policy. There is no Department of Health Law and Policy at the university. That error has also been corrected.








