In 2006, Shinya Yamanaka of Kyoto University made a startling discovery. He found that when he introduced the genes for a set of four proteins into mouse skin cells, the cells became reprogrammed into ones that closely resembled embryonic stem cells. One year later, Dr. Yamanaka showed that the same four factors also worked to reprogram human skin cells. Known as induced pluripotent stem cells, these new cells have revolutionized the field of stem cell biology.
Indeed, in early 2010, the journal Nature Methods dubbed the process by which induced pluripotent stem cells are produced its “method of the year,” citing the promise the cells hold for regenerative medicine and drug discovery and development. Recognizing their biomedical potential, many research laboratories have jumped on the “induced pluripotent stem cell” bandwagon. But induced pluripotent stem cells offer more than just a biomedical breakthrough. As a substitute for embryonic stem cells, they neatly sidestep ethical dilemmas that have threatened to hold back this important area of research. Because of these ethical advantages, not only scientists but also leaders of the Catholic Church have embraced the possibilities they offer. Thus, both sides of a historically contentious stem cell debate appear to be on board with the new pluripotent stem cell technology.
Unfortunately one residual ethical problem remains: Induced pluripotent stem cells still have to be tested and validated using embryonic stem cells, at least in these early stages of their experimental development. During this critical juncture, constructive dialogue between the two sides of the debate is vital to ensure a quick and ethical transition to a new era in which embryonic stem cells are no longer needed for research.
The Ethical Advantage
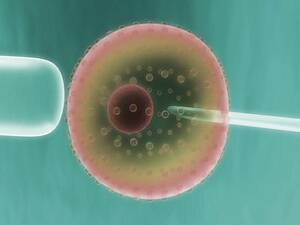
There are at least three strong ethical advantages to pursuing induced pluripotent stem cell technology. First and foremost, the production of such stem cells does not involve the destruction of human embryos. Rather, the reprogramming process by which induced pluripotent stem cells are made involves the conversion of a somatic (body) cell—that is, a cell that has already developed into a specific part of the body, like a skin cell—back into a malleable stem cell that can grow into any part of the body. This is in contrast to the situation involving the isolation of embryonic stem cells, which are extracted from the inner cell mass of embryos produced through in vitro fertilization in a process that inevitably destroys the embryos.
That leads to a second ethical advantage of induced pluripotent stem cells. Since in vitro fertilization is not involved, women’s eggs are not used, and all the ethical issues associated with the production and use of eggs for stem cell research, as well as with in vitro fertilization itself, are avoided. A third advantage relates to so-called therapeutic cloning, the transfer of the nucleus of a somatic cell into an egg from which the nucleus has been removed. The original rationale for therapeutic cloning was that it made possible the production of stem cells that are genetically (and immunologically) matched to the person who contributed the somatic cell nucleus. Such matching was not possible with embryonic stem cells because they came from a different individual—the embryo that contained them. But induced pluripotent stem cells are already matched because they come from the patients themselves—for instance, from skin cells obtained through biopsy. This renders therapeutic cloning unnecessary.
The use of induced pluripotent stem cells thus dodges the ethical dilemmas associated with embryonic stem cells. Embryos are not destroyed; in vitro fertilization is not required; and therapeutic cloning no longer offers any apparent advantage.
The Medical Promise
What is it that makes embryonic stem cells and the induced pluripotent stem cells that resemble them so compelling as tools in biomedical research? Unlike the cells of the adult body, embryonic stem cells and induced pluripotent stem cells have the ability both to continue to grow indefinitely in culture (self-renewal) and, when given the right signals, to morph into any of the cell types of the body (pluripotency). That means that embryonic stem cells or induced pluripotent stem cells grown in culture can be stimulated to change into specialized cell types outside the body, amplified in culture and then transplanted back to treat, for instance, spinal cord injury, Alzheimer’s disease or juvenile diabetes.
Any pluripotent cell, regardless of type, has this potential to be used in cell transplantation therapy. Like their embryonic counterparts, induced pluripotent stem cells have been shown to be capable of differentiating into a variety of cell types. Having an abundant supply of cells of various types (liver, kidney, heart) from different genetic backgrounds not only makes cell transplantation therapy possible, but it also facilitates the screening and development of new drugs. Moreover, unlike embryonic stem cells, induced pluripotent stem cells also can be used for “disease in a dish” studies—that is, they can be used in the laboratory to study disease progression. In these studies, the induced pluripotent stem cells originate from body cells of a patient who suffers from a particular disease. Several diseases—Lou Gehrig’s, Parkinson’s, spinal muscular atrophy, thalassemia and familial dysautonomia—already have been studied in this way.
Much of what we know about induced pluripotent stem cells has come from parallel studies done using mice. One of the most stringent tests for pluripotency involves the generation of mice through a process known as tetraploid complementation. Here, the fetus that is generated is derived entirely from the induced pluripotent stem cells. If the resulting mouse is viable and fertile, this demonstrates that the cells from which the mouse was formed were fully pluripotent. Recently, induced pluripotent stem cells from mice were shown to pass this most stringent test, indicating that induced pluripotent stem cells are equivalent to embryonic stem cells, at least in the mouse.
But tetraploid complementation cannot be done in humans since the individual produced would be a human clone, an ethical nonstarter. In its place, in human research, pluripotency can be tested by making detailed molecular comparisons that probe the functional equivalency between the induced pluripotent stem cells and their embryonic counterparts. It is this use of embryonic stem cells in such comparisons, of course, that accounts for the residual ethical problems that must be faced in the use of induced pluripotent stem cells.
Such final comparisons, however, are critical to biomedical progress. So far they have revealed that the induced pluripotent stem cells currently available are not exactly the same as embryonic stem cells, a result that, though disappointing, is not unexpected. Indeed, how likely is it that Dr. Yamanaka would have hit on exactly the right cocktail of reprogramming factors from the start? One would expect that some refinement of the original procedure would be necessary. Through intense and focused work, researchers now are gaining clues as to what those refinements will be. Fortunately there may be a way out of the ethical trap such laboratory comparisons appear to represent.
An Ethical Vaccination
In its instruction “Dignitas Personae” (“The Dignity of a Person”), issued in December 2008, the Vatican weighed in on a number of bioethical issues: in vitro fertilization, preimplantation genetic diagnosis, gene therapy, cloning and stem cells, among others. One issue it did not speak to was induced pluripotent stem cell technology. Despite this silence, “Dignitas Personae” does contain a framework for an ethical solution to the use of embryonic stem cells to validate induced pluripotent stem cells. In the section titled “The Use of Human ‘Biological Material’ of Illicit Origin,” which is concerned with the use of vaccines derived from cell lines obtained from past abortions, the Vatican document says that “danger to the health of children could permit parents to use a vaccine which was developed using cell lines of illicit origin, while keeping in mind that everyone has the duty to make known their disagreement and to ask that their health care system make other types of vaccines available.”
Applying this same logic, it may be ethically acceptable for someone to benefit from therapies or treatments derived from induced pluripotent stem cell lines that were validated by comparison with embryonic stem cells as long as that person makes known his disapproval of embryonic stem cell research. The person in this case would not be morally complicit in the original act of destroying the human embryo from which the embryonic stem cell line was obtained. A key component of this rationale, however, is the assumption that there is no continuing program of embryo destruction.
It is an unfortunate fact that if induced pluripotent stem cell technology succeeds, it will have done so in part at the expense of human embryos. There are as many as 700 human embryonic stem cell lines in existence worldwide. Each of these lines is associated with the death of a human embryo, a human individual. James Thomson, the University of Wisconsin biologist who not only helped pioneer the creation of induced pluripotent stem cells but also in 1998 was the first researcher to isolate embryonic stem cells from human embryos, has said that “if human embryonic stem cell research does not make you at least a little bit uncomfortable, you have not thought about it enough.” We should be uncomfortable, and we should do everything in our power to minimize human embryo destruction.
Building Constructive Dialogue
Historically, the embryonic stem cell debate has been cast in terms of a conflict between pro-life advocates on one side and scientists and medical researchers on the other. With the advent of induced pluripotent stem cell technology, however, the debate has entered a new phase. Both sides now want this technology to succeed. Most pro-life advocates see induced pluripotent stem cell technology as an ethically acceptable alternative, and they want to encourage it. Medical researchers also want the technology to succeed because induced pluripotent stem cells not only are free of the ethical baggage of embryonic stem cells, they are also much easier to generate in the laboratory. This shared desire for success offers an unprecedented opportunity for constructive dialogue.
For that dialogue to succeed, concessions must be made on both sides. Scientists will need to assess whether additional embryonic stem cell lines are actually needed for the induced pluripotent stem cell validation and improvement process or whether the hundreds of lines now available are sufficient (as I would argue). As they go about answering this question, they should bear in mind that for many people each human embryo is a unique individual. By accommodating that viewpoint, scientists will begin to gain the respect of those who value embryonic human life. Showing this kind of good will toward the other side is important for making progress in the debate.
For their part, pro-life advocates will have to face the possibility that additional testing using embryonic stem cells may be necessary at this point in order to perfect the cellular reprogramming procedure at the heart of induced pluripotent stem cell research. But the disappointment this requirement brings is attenuated by the fact that embryonic stem cells from lines already derived can be used. Finally, Catholic leaders, in their desire to promote this ethical, more favorable stem cell technology, sometimes have made statements that are inaccurate—implying, for instance, that induced pluripotent stem cells are a type of adult stem cell. While induced pluripotent stem cells are derived from adult cells, it is not accurate to say that they are a type of adult stem cell. Unfortunately, misleading statements of this nature confuse a person not trained in the relevant sciences and undermine meaningful dialogue with scientists. Our leaders may want to be more careful in this regard.
Research by means of induced pluripotent stem cell technology already is transforming the medical and bioethical landscape. It holds great promise in the areas of regenerative medicine, the study of disease progression and the development and testing of drugs. The key to a rapid and successful transition to a new era in which embryonic stem cells are no longer needed will be clear-headed and honest dialogue among all participants in this previously intractable debate.
Listen to an interview with W. Malcolm Byrnes.








If the development of these stem cells forestalls the need for therapeutic cloning, then the days of destroying blastocysts for this purpose are over. Stem cells derived from blastocysts (they are not "embryos" prior to gastrulation) had the problem of being untried by having gone through gastrulation - which is the point at which mother nature proves that the embryo is somewhat viable. The new pluripotent stem cells have already been screened by gastrulation - so we know they meet that test.
I do not share the ethical qualms of some on using cells derived from blastocysts, primarily because ensoulment can not be demonstrated prior to the commencement of regulative development. During generative development (prior to gastrulation) twining can occur and more importantly, non-human hybrids can continue to grow. Unless Heaven is filled with failed blastocysts, including those with only one human parent, it is not reasonable to conclude that ensoulment takes place prior to gastrulation.
Stem cell research prior to gastrulation actually proves that gastrulation is the key marker for ensoulment. Prior to this point, stem cells are harvested by removing the proto-Chorion. No cells that would become human beings are harmed. Indeed, given the right nutrition, they are ontologically identical to pluripotent stem cells derived in the new process (except, as I stated, they are less likely to be viable for not having been through gastrulation). A thought experiment confirms why there is no ethical difficulty in destroying a blastocyst. I call it stem cell harvesting in reverse. Imagine that stem cells were removed from a blastocyst and replaced with pluripotent stem cells created with the new process (assume no risk of rejection). Imagine further that the new combined blastocyst were implanted into a host mother and allowed to mature. The question to consider is, whose soul would the child have? Possible answers are A. It is a gollem with no soul. B. The original blastocyst, C. The stem cell donor. D. It's own. I would hope you would find the answer to be obvious, although if you didn't get D, you are wrong. If you did get D, however, you need to disregard the ethical concerns often raised about stem cell research using blastocysts.
This is a very well-written article-lucid, informative, and straightforward. But the key takeaway IMO comes down to this sentence: "We should be uncomfortable, and we should do everything in our power to minimize human embryo destruction." The rub for me is the word "minimize." Despite the great promise of induced pluripotent stem cell technology, the author makes what is essentially a utilitarian argument. Is the death of even one embryonic stem cell for research purposes-even if it is sacrificed for "comparison" purposes with a potential substitute-ever justified? Does the doctrine of necessity (including perceived necessity) permit the killing of a human being, which an embryonic stem cell certainly is? The author is rightfully squeamish about what he proposes, even if the comparison to be made involves embryonic stem cell lines already in existence. And suppose, in the end, Dr. Yamanaka wasn't able to "hit exactly on the right cocktail of reprogramming"? The destruction of embryonic stem cells in the attempt would have been doubly in vain.
A blastocyst is not an organism, simply because it has no organs. It is unorganized potential human life. It does not have integrity - meaning you could evacuate half the stem cells and let the other half mature and not damange the bodily integrity of the child. That is a strong indication that it is not a "being" and that efforts to call it one have more to do with doctrinal consistency than truth. We need not back the hierarchy's position when it is clearly in error. Unquestioned loyalty is bureaupathology, not faith.
"Essential humanity" and "potential human life"...Those are extremely slippery slopes and utilitarian to the core. And no need to bring in ensoulment. I was making a nonsectarian argument only as to what constiutes a human being.
You and I are the products of the fusion of human gametes, one from each of our human mothers and one from each of our human fathers. What would the offspring of human parents be but human beings? No technical definition is needed for beingness: We're beings because we exist. And we're human throughout the continuum of our existence-from fertilization to death-because we have the DNA complement of members of the human species. Certainly you're not saying that there was a period in your continuum of physical existence that you were not a human being? I'm not willing to concede that about myself. :)
Even some of the most ardent pro-choice moral ethicists (e.g., Peter Singer) rightly concede that a human being exists at conception. They instead move on from their concession to address the issue of when a human being becomes a person. For myself, that's a non-issue. Every member of the species homo sapiens is entitled from the first moment of its existence to protection because of its inherent human dignity, regardless of the debate about the timing of when a human being is dubbed with the legal term "person." Legal definitions are inexact and open to modification and retraction; they have their place, but I think the moral argument regarding embryonic stem cells best rests on an inherent human dignity foundation.
Facts are never utilitarian, Bill. I was not me until I was fully my father's son - and that happened at gastrulation. If science shows that this really is a vitally important marker on what is and is not personhood, then moral philosophy should conform to it - not the other way around. Ontologically, there is nothing which supports conception over gastrulation. Indeed, if the essential parts of you are what you consider in this analysis, you must concede that part of the blastocyst (the part that is destroyed in the harvesting of stem cells) isn't even you - it is or will be the afterbirth. The fact that the stem cells don't die when the chorion is removed is proof that the stem cells are not essentially different than any other biological sample.
The thing is, by acknowledging that it might be necessary to create and destroy more embryos in order to measure IPSC results (even though he personally does not believe so), he doesn't quite close the loop on the loophole he seeks to create.
Perhaps a pro-life scientist can make IPSC's available without such measurement. The presence of a serious affliction might allow one to legitimatley accept un-tested IPSC's, which would be an acceptable risk to the patient.
The scenarios that Dr. Byrnes puts forth allowing Catholics to use IPSC's even with embryonic stem cells as part of the general IPSC program (e.g.: NO MORE embryonic cells are currently being destroyed and we register disapproval of their use) seem "wink and nod" at best. The first part, just plain unlikely.
It's this sort of, "Doctor, I disapprove... but give me the shot anyway," that provides just the type of fodder for those who seek to lampoon people of faith that they live for.
Of course, one must, wiithin guidelines, use his or her prudential judgment when faced with such situations, to the extent allowed.
Please, keep publishing such articles. These types of issues can never be clarified or refined enough.
We must not forget that we as the Church hold it also morally wrong to CREATE embryos artificially. In vitreo fertilization, even for the purpose of allowing a new life that will be loved and wanted to result, is thus wrong.
We have to remember ALL components of an issue.
Keep the discussion going!